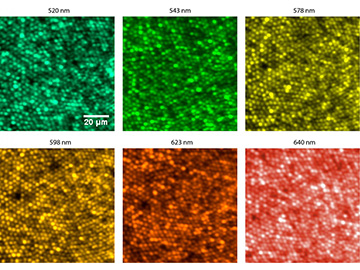
False-color images of the fovea, or retinal focusing center, captured at different wavelengths using a new system that compensates for longitudinal chromatic aberration in ophthalmic instruments. Each bright dot in the image is an individual retinal photoreceptor, or cone, around 2 microns in diameter. [Image: Xiaoyun Jiang, Ramkumar Sabesan, University of Washington] [Enlarge image]
The human eye, like other optical devices, isn’t perfect. As a result, designers of ophthalmic instruments for the clinic and elsewhere need to find ways to compensate for the eye’s optical aberrations, which differ from patient to patient, to get a clear reading. To do so, those designers have relied on adaptive optics, the same techniques that allow astronomers to cancel out the blurring effects of Earth’s atmosphere and see the stars beyond.
But adaptive-optics schemes tend to cancel only aberrations that aren’t wavelength dependent—and chromatic aberrations, whose effects differ depending on the wavelength involved, have been much tougher to assess and rein in. Now, a team from the University of Washington (UW), USA, has devised a system that can compensate for longitudinal chromatic aberrations (LCAs) in imaging the retina (Optica, doi: 10.1364/OPTICA.6.000981). The researchers believe that the system could allow for better assessment of vision problems and performance, both in the clinic and the research lab.
Unique to the individual
LCA is a form of chromatic aberration that occurs when light through a lens, such as that of the eye, focuses at a different distance from the lens depending on the light’s wavelength. (A second form, transverse chromatic aberration, involves wavelength-dependent shifts of light to different positions within the same focal plane.)
Like so-called monochromatic, or non-wavelength-dependent, aberrations, LCAs are unique to an individual eye. But whereas adaptive-optics techniques can be and are used in the clinic to individually correct for monochromatic optical aberrations, clinicians usually rely on population averages to approximate LCAs in patient retinal images. That’s a blunt instrument at best, and makes it hard to get a clear picture for individual patients. Making matters worse, even those average “typical eye” LCA estimates are based largely on subjective, and thus inconsistent, reports from patients and experimental subjects.
Modding a Badal optometer
A better system would allow correction of LCAs on a patient-by-patient basis, without recourse to corrections based on population averages. To get there, the UW team, led by Ramkumar Sabesan of the school’s department of ophthalmology, envisioned an LCA compensator that could, in effect, be snapped onto ophthalmic instruments such as adaptive-optics scanning laser ophthalmoscopes (AOSLOs).
To make that vision a reality, Sabesan’s team began with an already-existing device called a Badal optometer. This device, effectively a telescope with movable focal elements, allows vergence—the instrument’s effective refractive power, related to the inverse of the focal length—to be tweaked without changing image magnification. The Badal optometer thus lets the instrument’s operator introduce a controlled amount of defocus into a specific measurement.
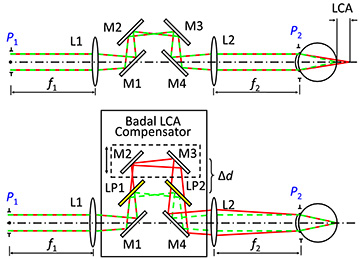
In a normal Badal setup, any two wavelengths of light will go through the same path length to the patient’s eye, where the eye’s LCA will force the wavelengths to be defocused with respect to one another. But Sabesan’s team cleverly modded the optometer by introducing a pair of long-pass filters into its visual path.
A conventional Badal optometer (top) passes light of multiple wavelengths through the same path length, leading to defocusing in the eye owing to the eye’s longitudinal chromatic aberration (LCA). The UW team’s modified optometer (bottom) includes a pair of long-pass filters, which allow the path length of one wavelength to be adjusted with respect to the other—and, thus, the eye’s LCA to be corrected for. M = mirrors; L = lenses; LP = long-pass filters. [Image: X. Xiang et al., Optica, doi: 10.1364/OPTICA.6.000981 (2019)] [Enlarge image]
In that setup, adjusting the Badal’s optics changes the path length of the longer wavelength while keeping the path length of the second, shorter wavelength constant. That, in turn, allows the defocus between that specific pair of wavelengths—and, thus, the patient’s individual LCA for that wavelength pair—to be measured and compensated for. And, by fitting the Badal optometer with a suite of different filters, the LCA compensation can be customized for an arbitrary set of wavelength pairs.
Counting cones
The UW team added their compensator to several different ophthalmic instrument setups, including an AOSLO and an adaptive-optics vision simulator, and then tested the setups out on a number of volunteer subjects. The team was indeed able to correct for LCA on a patient-by-patient basis—even to the point of gaining sharp images of the retina’s color-focusing center, the fovea, at multiple different wavelengths, each sufficiently sharp to count the individual cone photoreceptor cells.
The researchers believe that the system will prove useful not only in gaining high-quality retinal images at multiple wavelengths in the clinic, but also for studies of visual performance over time and with aging, as well as for efforts to understand different types of colorblindness. In a press release accompanying the work, Sabesan maintained that the system should facilitate “future investigations into how we see color in our environment, unimpeded by the native chromatic imperfections of the individual.”