A Duke University team used a simple laser setup to test 14 facemasks commonly used to prevent coronavirus transmission—and found significant differences in mask efficacy. [Image: photo by E. Fischer, Duke University, in E.P. Fischer et al., Sci. Adv., doi: 10.1126/sciadv.abd3083 (2020); CC By-NC 4.0] [Enlarge image]
COVID-19 has had many impacts on daily life—and among the most visible is the varied and sometimes creative approaches to facemask design that the pandemic has spurred. Citizens complying with worldwide mask mandates can be seen decked out in everything from professional surgical masks to home-stitched, brightly patterned cotton coverings to an ordinary bandana wrapped around the face. But—fashion aside—how effective are these improvised coverings at actually preventing spread of the disease?
A group at Duke University, USA, has developed a low-cost optical approach to provide some answers to that question (Sci. Adv., doi: 10.1126/sciadv.abd3083). The team’s straightforward setup involves an inexpensive laser, a dark box and a mobile-phone camera, coupled with a simple computer algorithm. The message of the team’s early mask tests using the setup is clear: All masks are not created equal—and some homemade masks may be worse than useless at stopping COVID-19’s spread.
Droplet threats
As many are aware at this point, the main role of facemasks is not to protect the wearer from COVID-19, but to keep the wearer from spreading the disease to others through virus-laden droplets. And it’s become increasingly apparent that infected individuals can spread such droplets not just by sneezing, but even in the course of ordinary speech and breathing.
One research strand that helped establish that risk was work reported earlier this year by scientists at the U.S. National Institutes of Health (NIH) and the University of Pennsylvania. In papers published in the New England Journal of Medicine and PNAS, the NIH–Penn team showed that the volume of droplets ejected during ordinary speech could be visualized through scattering of a sheet of laser light, as it passed through a simple cardboard box painted black, into which a test subject spoke.
Coincidentally, the Duke University researchers behind the new work, led by OSA member Martin Fischer, were in search of a way to test a particular mask prototype that the university was planning to buy in volume, for distribution to underserved communities in the school’s local area of Raleigh/Durham, NC. The team hit upon the idea of adapting the simple visualization scheme previously reported by the NIH–Penn group for testing the prototype COVID-19 masks.
Laser, lens, box and cellphone
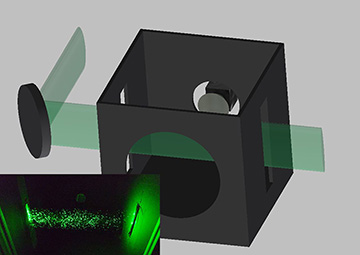
In the team's test setup, a laser beam, passed through a cylindrical lens to create an elliptical profile, is shone through slits as a light sheet into a black box. A mask-wearing test subject speaks through the hole in the front, and video of droplets scattering off of the laser sheet is captured by a cellphone camera at the back. Inset shows a sample image of water scattered from a spray bottle. [Image: E.P. Fischer et al., Sci. Adv., doi: 10.1126/sciadv.abd3083 (2020); CC By-NC 4.0] [Enlarge image]
The mask-testing setup, as Fischer noted in a Q&A accompanying the research, is “much simpler than those commonly seen in typical laser labs: it consists only of a laser, a lens and a camera.” Specifically, a laser is shone through a cylindrical lens to create an elliptical beam profile, which then passes through a slit into a 30×30×35-cm black box, creating a light sheet within the box.
To put a mask to the test using the setup, a person wearing the mask speaks into a hole cut in the front of the box; through another hole in the back, a mobile phone records video as the laser light scatters off of droplets coming from the speaker’s mouth. The video file is then piped to a computer algorithm, which counts the droplets recorded in the light scattering.
The team used one of the scientific lasers in the lab at Duke—a 2-W, 532-nm model from Spectra-Physics. But the researchers say that the setup should work equally well with cheap, commercially available lasers retailing for less than US$100. Indeed, they believe that the whole setup should be achievable for a total spend of less than US$200, and that it can “easily be built and operated by non-experts.”
Winners and duds
The team used the setup to test 14 “commonly available masks or mask alternatives,” ranging from gold-standard, professionally test-fit N95 masks and surgical masks to hand-sewn knitted and cotton varieties, fleece neck wraps and bandanas. Each trial began with a control run, during which the test subject spoke the phrase “stay healthy, people” without wearing a mask, followed by a run with the face covering being tested. The test was repeated ten times for each mask under review.
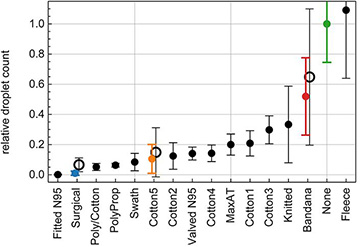
Plot of proportion of droplets allowed through by each mask tested, showing wide variation in efficacy among mask types. [Image: E.P. Fischer et al., Sci. Adv., doi: 10.1126/sciadv.abd3083 (2020); CC By-NC 4.0] [Enlarge image]
Some of the results weren’t terribly surprising. For example, the professional-grade N95 masks (without exhaust valves) were the most effective, allowing less than 0.1% of droplets to pass through. Surgical masks also effectively blocked most droplet transmission. Commercial and homemade cotton masks were less effective, but in most cases still held back 80% or more of droplet transmission—far better, certainly, than wearing no mask at all.
The performance of other materials, however, was more problematic. Bandanas, for example, allowed an average of more than 50% of droplets through (with a wide variance). And the tests suggested that one popular homemade mask solution—covering the face using a fleece neck wrap (such as a balaclava)—may actually increase the number of small droplets transmitted. The team speculated that that might be because the fleece material breaks larger droplets down into smaller ones that pass through.
The team also warned against the use of masks with an exhaust valve (even N95 masks). Such masks have become popular because they are more comfortable to wear. But Fischer said that, perhaps not surprisingly, they “do a great job of protecting the wearer from the outside environment, but a bad job of protecting others from the wearer.”
A community solution?
The researchers acknowledge that their testing setup has some limitations. For example, the laser light sheet, which covers only a limited area, may not be registering all droplets in the box. Also, the positioning of the speaker with respect to the box varies from person to person, so it may be difficult to compare results of different speakers. The detection sensitivity and resolution of the mobile-phone camera also injects an element of uncertainty. Some of these disadvantages, the authors suggest, could be overcome by tweaking the setup in a variety of ways.
Nonetheless, the team believes that the simplicity and straightforwardness of the setup they present trumps these disadvantages, by offering a low-cost tool that communities can use to educate the public and that mask producers can use to verify efficacy. Fischer does note, however, that the team’s specific setup, which relied on a high-power scientific-grade laser, requires some precautions for eye safety, and would need to be set up by someone with at least some laser training. “We are working on a design that uses a lower-power, eye-safe laser,” he says.