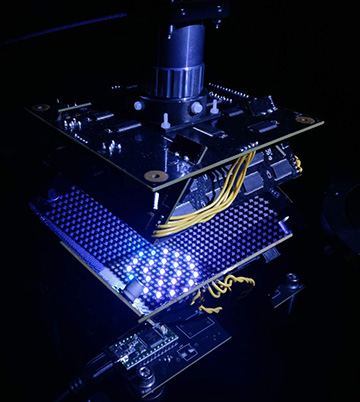
U.S. and German engineers have developed a microscope that uses machine learning to co-optimize illumination from a bank of 1,500 programmable LEDs and image classification, for faster diagnosis of malaria. [Image: Roarke Horstmeyer, Duke University]
Nearly half the world’s population is at risk of malaria, with an estimated 219 million cases of the mosquito-borne disease in 2017 alone, according to the World Health Organization. Early and accurate diagnosis of malaria allows clinicians to treat infected individuals quickly, which increases their chances of survival and prevents further transmission of the disease. Researchers in the United States and Germany have now brought optics and machine learning together in a bid to accelerate the disease’s diagnosis (Biomed. Opt. Express, doi: 10.1364/BOE.10.006351).
Clinical bottlenecks
The most common diagnostic test for malaria involves examining a drop of blood under an optical microscope to check for the presence of Plasmodium falciparum, a single-celled parasite that causes malaria. It can take an expert 10 to 15 minutes of manually scanning around a single slide to come to a definitive conclusion. That can create a severe bottleneck at clinics with many patients and few trained professionals.
To speed up the diagnosis pipeline, the researchers behind the new study have added the one-two punch of machine learning and a programmable LED array to a standard light microscope. The team’s modifications enable the “smart” microscope to find the ideal LED illumination pattern for rapid and accurate detection of the parasite. It then uses a deep neural network to automatically classify the resulting image as infected or uninfected. The entire process takes no more than ten seconds.
Sparsely populated samples
“The idea for this application arose when I met co-author Barbara Kappes [of Friedrich-Alexander University], who works with malaria, while I was a postdoc in Germany,” said Roarke Horstmeyer of Duke University, the new study’s corresponding author. “She explained the challenges that clinicians currently face when looking at a slide to detect malaria infection. It seemed like a natural fit to optimize the properties of the microscope itself for this task.”
The gold standard for malaria diagnosis in resource-limited settings is a light microscope with a high-resolution, oil immersion objective lens. Such a lens commonly has a very limited field-of-view that will only contain a few dozen cells. Because P. falciparum parasite tends to be quite sparsely distributed in a given sample, a clinician must scan through 100 or more unique fields of view for a confident diagnosis.
Optimizing lighting and image classification
Horstmeyer and his colleagues took the opposite approach with their prototype microscope, using a large-field-of-view, low-resolution objective lens to capture thousands of cells in one snapshot. Even a well-trained human eye—or a machine-learning algorithm—wouldn’t be able to pick out the micron-sized microorganism at this point.
It is here that the microscope’s programmable LED array comes into play, applying just the right lighting pattern to highlight the presence of a parasite. The researchers used an enhanced convolutional neural network to train the microscope to control the brightness and color of the 1,500 LEDs arranged in a bowl-like geometry to surround the sample from below.
Accuracy jump
The approach allowed the system to learn the optimal illumination scheme to maximize image classification accuracy. In the end, the algorithm favored high-angle illumination along with a ring-shaped pattern of different colors. The prototype microscope demonstrated greater accuracy than trained physicians and other machine-learning algorithms, the accuracy for which typically hovers around 75%.
“We’re in the area of 95% to 99% classification accuracy while seeing a thousand cells all at once,” said Horstmeyer. “Now we’re working toward our goal of taking our research into a real diagnostic setting by miniaturizing the microscope and setting it up in partner pathology labs in India.”
In addition to researchers at Duke University and Friedrich-Alexander University, the team also included scientists from Y Combinator Research, USA, Charitè Universitätsmedizin and Humboldt University, Germany, and Fraunhofer IISB, Germany.
