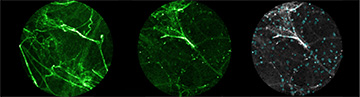
Left: Tissue strands in the lung of a patient with suspected bronchiectasis. Center: The patient once the chemical probes have been sprayed into the lung, causing the bacteria to glow and create a “snow-like” twinkling effect on the screen. Right: Data after image analysis techniques. [Image: University of Edinburgh]
Lung infections due to Gram-negative bacteria are notoriously difficult to diagnose rapidly for prompt treatment. A new procedure involving an optical probe and a fluorescent marker could make those pulmonary predators pop out on a display screen, leading to rapid diagnosis of potentially deadly pneumonia (Sci. Transl. Med., doi:10.1126/scitranslmed.aal0033).
The researchers at the University of Edinburgh, Scotland, U.K., who developed the in situ optical-identification technique have already tested it on human patients, as well as in animal tissue.
Engineering a fluorescent marker
So-called Gram-negative bacteria—the name comes from their lack of reaction to a crystal violet stain—have an outer cell membrane that contains an endotoxin with a component called lipid A. In small amounts, lipid A can provoke an attacking response from the human body's immune system, but higher concentrations during an infection by Gram-negative bacteria can lead to septic shock, and even death, in the patient. Traditional methods for diagnosing Gram-negative pulmonary infections, from lung-tissue biopsy to sputum cultures that take days to produce results, have significant drawbacks.
To get around those drawbacks, the Edinburgh team sought a fluorescent marker that would adhere specifically to Gram-negative bacteria. They found that an antimicrobial peptide called polymyxin selectively binds to the lipid A in the outer membrane of Gram-negative bacteria. Then, they attached the polymyxin to a fluorophore molecule. By testing the combination marker on several species of disease-causing bacteria, the scientists found that the marker produced fluorescent amplification with good signal-to-noise ratios when it hooked up with Gram-negative bacteria, but not with Gram-positive pathogens. The marker also distinguished between bacteria and mammalian cells in vitro.
Animal and human testing
After toxicology tests to make sure that the fluorescent marker did not damage animal tissues, the team hooked up ex vivo sheep lungs to a mechanical ventilator. The researchers then tested the ability of their optical endomicroscope with an optical-fiber probe to detect the bacteria's fluorescence within tissues. The fluorescence confocal endomicroscope captured images at 12 frames/s and used a 488-nm laser as the illumination source.
Finally, the researchers used their system on two small groups of humans: six patients with bronchiectasis, a chronic condition of airway enlargement with mucus production leading to frequent infections, and seven mechanically vented patients who were in the intensive care unit with suspected pneumonia. The clinical version of the optical endomicroscope had a circular field of view roughly 600 μm in diameter. Image-processing algorithms made the Gram-negative bacteria appear as bright spots.
