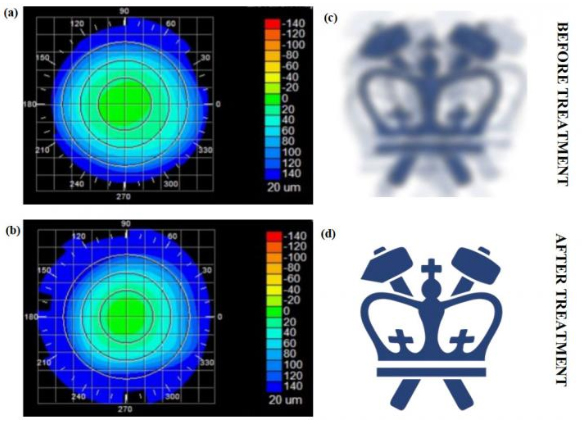
Corneal topography before and after the Columbia team’s fs laser treatment, paired with “virtual” vision simulating the effects of the induced refractive-power change. [Image: Sinisa Vukelic/Columbia Engineering]
By 2020, some 2.5 billion people worldwide may be affected by myopia, or nearsightedness. Corneal refractive surgery has emerged in recent decades as a more permanent fix for the condition than glasses or contact lenses—but vision surgery is invasive, and subject to post-surgical complications and even vision loss in rare cases.
Now, a research team at Columbia University, USA, has developed a noninvasive technique that it says can permanently correct vision (Nat. Photon. doi: 10.1038/s41566-018-0174-8). The method relies on a low-powered ultrafast laser and photochemical effects to alter biochemical and biomechanical properties of corneal tissue. According to the researchers, this nonsurgical technique, which has fewer side effects and limitations than refractive surgeries, could lead to treatment for myopia, hyperopia, astigmatism and irregular astigmatism.
Looking past LASIK
Laser-assisted vision correction surgeries such as laser in situ keratomileusis (LASIK) and photorefractive keratectomy (PRK) have high success rates, but the ablative technology, which can thin and even weaken the cornea, comes with risks and a number of reported side effects. Moreover, some patients (such as those with dry eyes, thin corneas and other abnormalities) are not good candidates for refractive surgery. As an alternative, Columbia Engineering researcher Sinisa Vukelic and his team propose a nonsurgical technique for permanent vision correction that reportedly avoids thermal ablation and optical breakdown.
The technique achieves those advantages through a different mode of laser–cornea interaction: it relies on a femtosecond oscillator that pulses very low energy at a high repetition rate to change the localized tissue’s macroscopic geometry. This kind of ultrafast laser lets the team use just enough power to induce low-density plasma (LDP), but not so much energy that the tissue is damaged. “This is a fundamental departure from the mainstream ultrafast laser treatment,” Vukelic explained in a press release, that “relies on the optical breakdown of the target materials and subsequent cavitation bubble formation.”
Building corneal crosslinks
The critical element of this approach is the induction of the LDP, which causes ionization of water molecules in the cornea. The ionization, in turn, creates a reactive oxygen species—an unstable molecule that contains oxygen and reacts easily with other molecules in a cell—which then interacts with the surrounding collagen proteins in the cornea to form crosslinks without the use of photosensitizers. The crosslinking alters collagen properties in the selected regions, resulting in changes to the cornea as a whole.
With this treatment, the team notes, only the targeted molecules are ionized, so optical breakdown of the corneal tissue is avoided. As the process is photochemical, tissue is not disrupted, and the induced changes remain stable.
Ex vivo and in vivo experiments
As a proof of concept, the team applied its method to pig eyes ex vivo, measuring the difference in corneal curvature, which in turn corresponds to the change in effective refractive power (ERP) after both corneal flattening and corneal steepening. (Corneal flattening is used to treat myopia; corneal steepening is a treatment for hyperopia, or farsightedness.) Over 24 hours, the team observed a strong change in ERP, followed by partial recovery and stabilization at about 3.45 diopters, on average.
After treatment, the team tested for laser-induced changes in corneal temperature, for corneal hazing and for changes in crosslink density. The researchers observed no laser-induced damage under standard histological examinations and confocal imaging—which, they suggest, confirms that the femtosecond laser treatment effectively changed the refractive power of the pig eye without adverse side effects.
The researchers followed up those ex vivo experiments with in vivo tests on rabbit eyes. Tracking changes in ERP regularly over three months after treatment, the team found that those changes remained stable for three months, with a relative change in ERP of about 1.94 diopters. Histological examination revealed no thermal damage to stromal tissue, confirming the safety of the treatment, according to the team. Confocal imaging of the rabbit eyes revealed no difference in cellular structure or density after laser treatment.
Non-ocular possibilities
According to Vukelic, this technique can be applied to other collagen-rich tissues and could potentially be used to treat non-ocular conditions, such as early osteoarthritis. The team believes that this method could widen the pool of eligible patients for permanent vision correction, as well as eliminate the post-surgical complications associated with LASIK and PRK. “We think our non-invasive approach has the potential to open avenues to treat or repair collagenous tissue without causing tissue damage," said Vukelic.
