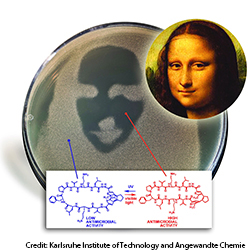
This bacterial culture contains an inactivated photo-switchable antibiotic. When scientists shine light through a mask shaped like the Mona Lisa's face, the antibiotic activates only in the regions exposed to the light.
A typical dose of antibiotics may come with side effects. However, researchers at two European universities have devised a light-activation mechanism to switch an antibiotic on and off, a process that could give physicians new treatment options for localized infections (Angew. Chem. Int. Ed. 53, 3392).
Researchers at the Karlsruhe Institute of Technology (Germany) and the Taras Shevchenko National University of Kiev (Ukraine) studied the properties of diarylethenes, a class of organic compounds that undergo reversible isomerization when exposed to light. Isomers are molecules that have the same molecular formula but different arrangements of their atoms. Diarylethenes have been studied elsewhere as potential switches in molecular electronics.
The team, under Karlsruhe professor Anne S. Ulrich, used a diarylethene as a building block called a “peptide mimetic.” The molecule stays in its “closed” form until it absorbs light energy, when it changes into its “open” isomer. The researchers incorporated the peptide mimetics into gramicidin S, a broad-spectrum topical antibiotic discovered in the 1940s. With the additional peptide, the modified gramicidin S molecule looks like a ring with an extra chain structure on the side.
To test the photoactivation of the antibiotic, the researchers grew a laboratory culture of Staphylococcus bacteria, then treated it with the inactive form of the gramicidin. After covering the culture with a mask, they irradiated it with ultraviolet or visible light of 256 or 530 nm respectively. In both cases, the germs died where the antibiotic had been exposed to light and lived where no light had reached the drug.
The scientists hope that such photoactivated molecular switching action could lead to new “smart” therapies that target infected tissue without inducing systemic side effects.
